Clinical characteristics
• Ischaemic colitis is caused by interruption to the colonic blood supply that include thrombosis , bowel obstruction and trauma.
• Some Predisposing factors included as age,oral contraceptives,sickle cell disease and surgical ligation of the inferior mesenteric artery.
• Presents with acute lower abdominal pain and tenderness,usually out of proportion to the clinical signs.There may be rectal bleeding or diarrhoea.
• Most commonly affects the left side of the colon, especially at the splenic flexure where there is a watershed between the territories of the superior and inferior mesenteric arteries.The rectum is usually spared.
• May be a transient condition with spontaneous resolution over a few months. May lead to incomplete healing with smooth stricture formation. Severe disease can lead to colonic infarction,with a high associated mortality.
Radiological features
• AXR : plain film is often normal;however,gas within the colon may out line the characteristic thumb printing of thickened, oedematous folds seen in this condition.
• Barium enema : single-contrast instant enema may demonstrate thumb printing and ulceration associated with this condition.Adoublecontrast enema shows these findings more reliably but should be used with caution in anacutely ill patient.A smooth stricture maybe demonstrated on a delayed study.
Late-stage ischaemic colitis. Single-contrast barium enema demonstrates a clear zone of transition between normal and abnormal colon at the junction of the middle and distal thirds of the transverse colon.The proximal colon has normal mucosa and haustral pattern while the distal
segment is featureless and abnormally narrowed.
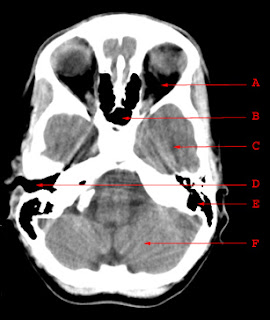
• CT :contrast-enhanced spiral CT is the usual first-line investigation for suspected ischaemic colitis.Adual phase scan,performed in the arterial and portal phases,may demonstrate thrombus in both the mesenteric arterial or venous systems.The affected colon may appear abnormally circumferentially thickened and demonstrate poor contrast enhancement.There may be a sharp cut off between normal and abnormal colon at the boundary of vascular territories.Mural gas may be seen in more advanced disease and,in severe cases,portal gas may be identified. The latter is a poor prognostic factor.
Superior mesenteric artery (SMA) thrombosis. Normal enhancement of the aorta (arrowhead). No enhancement seen in the SMA (arrow).
• Angiography :a more limited role in the era of multislice spiral CT but may demonstrate attenuated arterial flow or the presence of a thrombus.
Ischaemic colitis Clinical and Radiological findings